By Ahmed Sohaib Aslam, Niels H.Chavannes
Courtesy: Science Direct
Abstract
Physical activity (PA) is important for maintaining good physical health. WHO recommends 150 minutes of PA per week to the older population but many older people do not meet this recommendation. The increasing use of mobile technology among elderly provides an opportunity to increase PA. This systematic review was aimed at the usability, acceptability and effectiveness of mHealth (including smartphone, mobile phone, tablet apps, mobile text messages) to increase PA in older people above the age of 55. A literature search related to mHealth, PA and older people was conducted in PubMed, Embase, Web of science and COCHRANE library. The search generated 829 articles, after the screening of articles and reference lists, ten studies were included in the review. Included studies were diverse in the aspects of study design, intervention mode, duration, frequency of reminders and assessment measures. The results of this review indicated that mHealth interventions with motivational back up may be usable, acceptable and beneficial for the maintenance and improvement of PA in the short term. However, the findings are inconclusive about the difference in effectiveness between simple (mobile text message) and complex mHealth interventions (app monitoring with sensors), the optimal frequency for activity reminders and on the long term effectiveness of mHealth.
1. Introduction
Physical activity (PA) plays an important role in maintaining good physical and mental health(Warburton et al., 2006, Peel et al., 2005). However, the recommendation of the World Health Organization (WHO) of 150 minutes per week PA(World Health Organization. Global Strategy on Diet, Physical Activity and Health. https://www.who.int/dietphysicalactivity/leaflet-physical-activity-recommendations.pdfua=1. Published, 2011) is not met by the large number of older people(Sun et al., 2013) due to lack of interest (Satariano et al., 2000), lack of time (Dunn et al., 1999), decrease in work-related PA (Lahti et al., 2011, Slingerland et al., 2007), sedentary behaviour (Santos et al., 2012), fear of falling, difficulty in commuting to exercise gym or unawareness about the benefits of PA (Schutzer and Graves, 2004). Lack of PA is a major risk factor for adverse health outcomes across the life course(Lee and Lobelo, 2012). Among the elderly, it is a risk factor for cognitive decline, depression and disability(Lindwall and Hagger, 2011, Ávila-Funes and Aguilar-Navarro, 2011). Conversely, PA reduces the risk of disease (Pt, 2001, Sattelmair and Ding, 2011, Jeon et al., 2007, Monninkhof and Vlems, 2007, Wolin et al., 2009) and all-cause mortality, also among the elderly(Woodcock et al., 2011). Engaging in PA also reduces the risk of falls (Gillespie and Gillspie, 2012) and cognitive decline(Sofi and Bacci, 2011) in the older population. As a result, specific recommendations for PA in old age have begun to emerge(Nelson and Blair, 2007, Chodzko-Zajko and Fiatarone-Singh, 2009), yet most older adults do not meet these recommendations(Nelson and Blair, 2007). A systematic review has found increasing age to be a factor for diminished PA(Bauman and Sallis, 2012). Older people tend to be less physically active than young people, and when they do engage in PA, its intensity is lower(Chodzko-Zajko and Fiatarone-Singh, 2009).
EHealth and mHealth are technological advancements which could be helpful in promoting PA. The WHO defines eHealth as, “ the use of information and communication technologies (ICT) for health” while mHealth as, “the use of mobile wireless technologies for public health” (World Health Organization. https://www.who.int/ehealth/about/en/. Published, 2016). So, eHealth is a broader term related to telemedicine or telehealth (including mHealth) while mHealth is related to the mobile phone (Davis et al., 2016). EHealth and mHealth have novel solutions for guiding, training, motivating and reminding a person to engage in PA or exercise. The reminder for PA might be in the form of mobile text messages, pop-up screen reminders of an app, activity monitoring and advice for mobility besides the traditional methods of printed material, prescription, group training for exercise, face to face advice or the word of mouth (Marcus et al., 2006). MHealth might be the future of healthcare due to the increase in the use of mobile or smartphones and easiness of use (Lee, 2016). A mobile phone can remind people about the time for an activity, it can provide pop-ups to notice inactivity or boost up for achieving an activity goal. The scope of mHealth ranges from a simple mobile text message to a complex software/app and is useful for goal setting, coaching, monitoring and self-evaluation of exercise or activity. It might act as a tool to encourage people to perform PA which might range from a simple walk to any designated/specific exercise(O’Reilly and Spruijt-Metz, 2013, Gotsis et al., 2013). MHealth has some benefits; it is accessible everywhere and a person does not necessarily need a specific time and place to start exercising(California, 2010). Further, it is not necessary to consult a physical trainer in person (Geraedts et al., 2013).
Research findings on the effectiveness of eHealth (including mHealth) for PA in the general population are mixed and reviews report modest effectiveness of such interventions (Romeo et al., 2019, Coughlin et al., 2016, Flores Mateo et al., 2015). A systematic review has shown that eHealth (including mHealth) may be effective and acceptable to improve PA in people with a mean age of 55 years and above (Muellmann et al., 2018). The narrative review of Jonkman et al. (2018) also found that eHealth interventions measuring PA in the form of pedometers and accelerometers are effective in older people (Jonkman et al., 2018). However, a systematic review is lacking on the effectiveness of mHealth in older people to improve PA despite the growing increase in the use of mobile phones and smartphones.
This systematic review aims to study the effectiveness, usability and acceptability of mHealth for promoting PA in older people above the age of 55. As far as we know, this is the first review on the effectiveness of mHealth interventions on promoting PA in older people.
2. Methods
2.1. Search Strategy
An initial and updated literature search was conducted on August 20, 2018 and December 20, 2019 respectively, using the combination of key terms related to mHealth/eHealth, exercise/physical activity and older people in the databases of PubMed, Embase, Web of science and COCHRANE library. The search terms, MeSH and index terms, are attached in Appendix A.
3. The reference lists of the studies meeting the inclusion criteria and published reviews on eHealth to improve PA in older people were searched to find additional articles.
3.1. Inclusion and Exclusion Criteria
All study designs were included in this review. Studies were included in the review, if they met all of these three conditions, (1) age of all participants was 55 years or above, (2) mHealth as an intervention for PA, (3) the outcome measure was related to usability, acceptability and/or effectiveness on PA.
Regarding the second criterion, studies with mHealth interventions in the form of mobile phone, smartphone or tablets (text messages, mobile phone or tablet enabled software or apps and smartphones with or without portable activity monitors) targeting PA solely or as part of another treatment (e.g. in diabetic management) were included in this review.
Studies on telephone interventions, video callings, Personal digital assistants (PDAs) and web apps were excluded if it was not clear whether mobile phones/tablets were included in the intervention or not.
Studies not fulfilling any of the above conditions, letters to the editor, conference abstracts and reviews were also excluded.
3.2. Selection of studies
As a first step, the titles and abstracts screening of the literature was carried out by two independent authors (first and third author). In the second step, full-text articles of the relevant studies were screened while in the third step, the reference lists of the suitable articles and the review articles on eHealth were searched for additional articles. At each step, any disagreement was discussed until consensus was reached. In the case of non-consensus, the study was discussed with the second author and disagreements were resolved.
3.3. Data Extraction
A protocol was developed for data extraction from the articles. The information related to article (year of publication and country of research), participants (male and female ratio and mean age), intervention (name and description of intervention, duration and frequency of reminders for PA), research design, PA measures and results (effectiveness, usability and acceptability of the intervention) was extracted.
3.4. Study Quality
The quality of studies was assessed by two authors (first and third author) with Cochrane Collaboration’s tool for assessing risk of bias (Higgins et al., 2011) which has six domains: (1) sequence generation for random allocation to conditions; (2) concealment of allocation to conditions; (3) addressing incomplete outcome data; (4) selective outcome reporting; (5) blinding of participants and researchers, and (6) other sources of bias. Domain five was not applicable in this review as participants and researchers were aware of allocation to conditions. Therefore, this domain was not assessed. Each study received a judgement in the form of low risk of bias (+), high risk of bias (−) or unclear risk of bias (?) on respective domains.
The overall risk of bias was rated as low, if the study scored low risk of bias on three or more domains, moderate when it scored low on two domains and high when it scored low on one or no domain. If a domain was not applicable (N.A.), it was considered having a high risk of bias.
When the design of a study was not clear, the corresponding author was contacted through email for the details of the study design.
3.5. Data synthesis
We conducted a systematic review because quantitative data synthesis (meta-analysis) was not possible due to the low number of studies and heterogeneity of the data.
4. Results
4.1. Identified studies
The process of study selection for this review is summarized in figure 1. The literature search resulted in 662 articles after the removal of 167 duplicate articles, and 611 articles dropped out in the screening process. The major reasons for drop out of articles were the low age of participants, the lack of a mHealth component or the absence of usability/acceptability/effectiveness on PA. Only nine articles met the inclusion criteria and one article was found in the reference list of an eHealth review, so ten articles were included in this review.
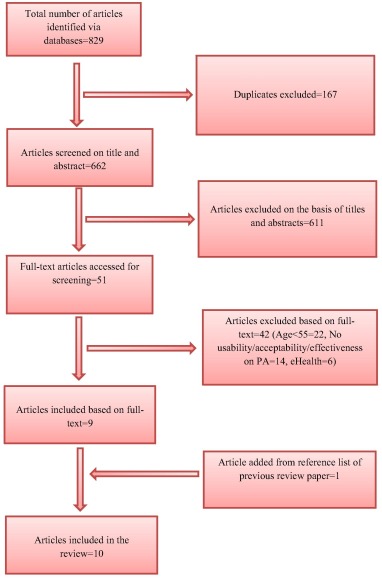
Figure 1. PRISMA flow chart diagram for the selection of studies
4.2. Study Quality
The assessment of study quality is presented in Table 1. The overall risk of bias was low in four of the studies and high in six of the studies. The risk of bias in the sequence generation and allocation concealment related to selection bias was low in four of the studies and high in six of the studies as the participants were not randomly assigned to the groups in most of the studies. The criterion of incomplete outcome data related to attrition bias scored low in most of the studies as the dropout of participants was low. While the information on selective reporting and the possibilities of other biases were rated unclear in the studies as it was often not reported.
Table 1. Summary of risk of bias assessment of included studies
| Study and study design | Random sequence generation | Allocation concealment | Incomplete outcome data | Selective reporting | Other bias | Summary risk of bias |
|---|---|---|---|---|---|---|
| Lyons et al., 2017 (Lyons et al., 2017)(RCT) | + | + | + | + | ? | + |
| Muller et al., 2016 (Muller et al., 2016)(RCT) | + | + | + | ? | ? | + |
| Knight et al., 2014 (Knight et al., 2014)(RCT) | + | + | + | ? | ? | + |
| Kim & Glanz, 2013 (Kim and Glanz, 2013)(RCT) | – | – | + | ? | ? | – |
| Joosen et al., 2018 (Joosen et al., 2018)(Pre-post randomized) | – | – | + | ? | ? | – |
| Hong et al., 2015 (Hong et al., 2015)(Pre-post study) | – | – | + | ? | ? | – |
| van Het et al., 2014 (van Het et al., 2014)(Pre-post with partial randomization) | – | – | + | ? | ? | – |
| Paul et al. (2017)(Paul et al., 2017)(Mixed method) | – | – | – | ? | ? | – |
| Shake et al, 2018(Shake et al., 2018)(RCT) | + | + | + | ? | ? | + |
| Li et al, 2019(Li et al., 2019)(Pre-post Test Pilot feasibility study) | – | – | + | ? | ? | – |
+ Low risk of bias, − High risk of bias, ? Unclear risk of bias
The study design was not clear in two studies and the corresponding authors of the studies did not respond satisfactorily to query and reminders.
4.3. Study and Intervention Characteristics
The characteristics of the included studies, studied populations, interventions and results are summarized in Table 2. The total number of participants in all studies was 383, of which 72% was female. The number of female participants was higher than the number of males in all studies except for one study by Joosen et al. (2018) with 8 female participants (40%). The average age of participants was 70 years, ranging from 61 years (Lyons et al. 2017) to 81 years (Joosen et al. 2018).
Table 2. Characteristics of studies, interventions, studied populations and results
| Study | Lyons et al., 2017 (Lyons et al., 2017) | Muller et al., 2016 (Muller et al., 2016) | Knight et al., 2014 (Knight et al., 2014) | Kim & Glanz, 2013 (Kim and Glanz, 2013) | Joosen et al., 2018 (Joosen et al., 2018) | Hong et al., 2015 (Hong et al., 2015) | van Het et al., 2014 (van Het et al., 2014) | Paul et al, 2017(Paul et al., 2017) | Shake et al, 2018(Shake et al., 2018) | Li et al, 2019yyy(Li et al., 2019) |
|---|---|---|---|---|---|---|---|---|---|---|
| Country of Study | USA | Malaysia | Canada (North America) | USA (African American descent) | Belgium | USA | Switzerland | UK | USA | USA |
| Study Design | RCT (Pilot) | RCT | RCT | RCT (Pilot) | Pre-post randomized | Pre-post | Pre-post (Preclinical exploratory with partial randomization) | Mixed methodspilot study | RCT | Pre-post Test Pilot feasibility study |
| N | 40 | 43 | 45 | 36 | 20 | 26 | 44 | 16 | 105 | 8 |
| Control (n) | 20 | 21 | N..A. | 10 | N.A. | N.A. | 17 | N.A. | 45 | N.A. |
| Treatment (n) | 20 | 22 | 45 | 26 | 20 | 26 | 27 | 16 | 60 | 8 |
| Female/Male | 34/6 | 32/11 | 25/20 | 29/7 | 8/12 | 18/8 | 28/16 | 8/8 | 90/15 | 6/2 |
| Mean Age (Years) | 61 | 63 | 63 | 70 | 81 | 69 (Median age) | 75 | 71 | 73 | 74 |
| Intervention | App & telephonic counselling | Motivational text message | Smartphone & Pedometer | Motivational text message | Smartphone & activity sensors | App | App | App | App | Smartwatch paired with tablet |
| Control Group | Waiting list control | Exercise booklet | N.A. (only intervention groups) | Walking instruction manual | N.A. | N.A. | Training plan diary | N.A. | Without exercise instruction | N.A. |
| Frequency of reminders (or use of intervention) | Encouragement to look at the goals and perform PA twice a day | Single Motivational text message a day for 5 days a week. | N.A. | Three motivational text messages a day, 3 days a week. | Sensors mounted on participants 8am-5pm for 5 days excluding weekends | One email after two weeks. | Daily Alarm reminder for exercise thrice a day. | Daily automatic | App use twiceper week foraround 1 hour | – |
| Duration (weeks) | 12 | 24 (text messages were used in first 12 weeks) | 12 | 6 | 10 | 8-12 | 12 | 6 | 10 | 4 |
| Studied Parameters | a) Acceptability & effectiveness of the appb) Step countc) Stepping time per day | a) Exercise frequency measured with exercise log.b) Secondary Outcome measurements (daily sitting time, Grip Strength, chair-stand test) | Step Count | a) Step Countb) Leisure Time Exercise Questionnaire (LTEQ) | a) Usability of smartphone for Automatic monitoring of PA behaviourb) Effects of mHealth system of activity sensors on PA | Effectiveness on goal setting for PA in cancer patients | Effectiveness for Exercise | a)Acceptability and usability of the appb) Step Count | a) Gait speedb) Chair stand and arm curl test for body strength | a)Sedentary timeb) PASE (Physical activity scale for the elderly) |
| Results | a) Acceptability was 4 on the scale of 5b) Increase of 1090 step count in intervention group in comparison to a decrease of 41 step count in control group after 12 weeks. Effect size was 0.26 (95% CI).c) Increase of 51 minutes in stepping time per day in the intervention group compared to a decrease of 2 minutes in control group after 12 weeks. Effect size was 0.35 (95% CI). | a) Increased exercise in intervention group compared to control group, when receiving text message in first 12 weeks (with mean difference of 1.21 and P=0.03).b) No significant difference from 12 to 24 weeks between control and treatment groups on secondary outcomes (P>.05). | Increase of 460 step count, not statistically significant (P=0.22) in sedentary group (advised to lower sedentary behaviour) while step count insignificantly decreased in exercise (advised for exercise) (p=0.84) and comprehensive (advised to avoid sedentary behaviour and do exercise) groups (p=0.19) after 12 weeks. | a) Increase of 680 step count in intervention group (P=0.05) in comparison to increase of 398 step count (P=0.23) in control group after 6 weeks.b) Improvement of 12 points in intervention group (P=0.001) in comparison to improvement of 4.6 points (P=0.01) in control group at LTEQ score after 6 weeks. | a) mHealth system practically work to automatically record the activity of a personb) Activity levels increased from week 1, peaked at week 5 and decreased slightly until week 10 on graphical display at automatic PA monitoring. | a)Number of participants engaged in regular PA increased by approx.16% (P=0.043).b)Participants completed 50% of the set daily PA goals (jogging, gardening etc.)c) Each participant completed 11 activities/goals. | Adherence to Strength-balance exercises for gait was 23% more in the tablet (active Lifestyle app group) than the brochure group. Gait quality was also improved in intervention group. | a)Acceptable to users and showed potential to increase physical activity in the interviews.b) Mean increase in step count =14%. , not statistically significant (p = 0.077); moderate effect size (d = 0.56) | a) The gait speedtest (4-meter walk)showed main effect of Time, F(1,83) = 8.71, P < 0.01, = 0.10,indicating that bothgroups improvedin gait speed.b) The exercise group performed better than only health education group in chair stand and arm curl tests. The arm curl test showed both a main effect of Time, F(1,81) = 11.40, P < 0.01, = 0.12, and a Group × Time interaction, F(1,81) = 4.78, P = 0.03, = 0.06. Pairwise t-test . The chair stand test showed a main effect of Time, F(1,77) = 13.18, P < 0.01, = 0.15, and a Group × Time interaction, F(1,77) = 4.20, P = 0.04, = 0.05. t-test comparisons indicated that the Experimental group improved, while the Control group did not. | a) Sedentary time decreased both during the intervention (D [mean difference] = −42.3 min, 95%CI[confidence interval] = [−79.4,−5.2], P = =0.03) and at post-intervention (D = −87.4 min, 95%CI=[−133.5,−30.4], P = <0.01).).b) The self-reported physical activity (PASE score) increased at the posttest (D = =96.2, 95% CI = [15.8,176.5], P = =0.025). |
| Outcome variable Assessment | 1.Baseline assessment one week before2. Midpoint assessment at 6 week3. Final at 12 week | At 12 and 24 weeks. | Each week. | Each week | Fitness test at the start, after 1,3,5,7 & 9 week, then after the 10 week. | Before and after the intervention | Baseline and after 12 weeks of the intervention. | Every week.. | Within one week before and after intervention | One week before, after 4 weeks of intervention and one week after the intervention |
| In and between group comparison | In & between intervention and wait-list groups | In & Between SMS receiving and non-receiving groups | In & between groups | In & between SMS receiving and non-receiving groups | Ingroup | Ingroup | In & Between tablet and brochure groups | Ingroup | In & Between only health education & exercise with health education group comparison. | Ingroup |
Of the ten studies, six were related to PA or exercise in community living healthy elderly (van Het et al., 2014, Lyons et al., 2017, Knight et al., 2014, Kim and Glanz, 2013, Muller et al., 2016, Paul et al., 2017), one to increase PA in older cancer patients (Hong et al., 2015), one to improve PA in healthy residents (chosen by a physiotherapist) of a care home (Joosen et al., 2018), one to senior centres (Shake et al., 2018) and one to the participants visiting a geriatric clinic (Li et al., 2019).
All of the ten studies investigated the effectiveness of mHealth and three studies examined features of acceptability and usability as well (van Het et al., 2014, Lyons et al., 2017)(Paul et al., 2017, Hong et al., 2015, Joosen et al., 2018). Tablet or mobile-enabled app interventions were investigated in five of the studies (van Het et al., 2014, Lyons et al., 2017)(Paul et al., 2017, Hong et al., 2015);(Shake et al., 2018) . Simple motivational text message interventions were used in two of the studies (Kim and Glanz, 2013, Muller et al., 2016). A smartphone with pedometer intervention was used in one study (Knight et al., 2014). A smartwatch paired with a tablet was used in one study (Li et al., 2019). While a mHealth system intervention (consisting of a smartphone with wireless activity sensor mounted on the body for automatic continuous monitoring of PA) was used in one study conducted at a care home (Joosen et al., 2018). The duration of use of the intervention was 12 weeks in five of the studies (van Het et al., 2014, Lyons et al., 2017, Knight et al., 2014)(Muller et al., 2016, Hong et al., 2015), 10 weeks in two studies (Joosen et al., 2018, Shake et al., 2018), 6 weeks (Kim and Glanz, 2013, Paul et al., 2017) in two studies and 4 weeks (Li et al., 2019) in one study. Post-intervention measurements were taken immediately or within one week after the end of the intervention period and there were no follow-ups.
Five of the studies were conducted in the USA, of which four included general older Americans (Lyons et al., 2017, Hong et al., 2015)(Shake et al., 2018, Li et al., 2019) and one included older immigrants of African descent (Kim and Glanz, 2013). The other five studies were conducted in Canada -North America (Knight et al., 2014), Belgium (Joosen et al., 2018), Switzerland (van Het et al., 2014), Malaysia (Muller et al., 2016) and UK(Paul et al., 2017).
Of the ten included studies, five studies were RCTs (Lyons et al., 2017, Knight et al., 2014, Kim and Glanz, 2013, Muller et al., 2016)(Shake et al., 2018), one was a pre-post randomized study (Joosen et al., 2018); two had a pre-post study design (Hong et al., 2015, Li et al., 2019), one was mixed-method study (Paul et al., 2017) and one had a preclinical exploratory design with pre-post measurements and a control group (van Het et al., 2014). There was no control group in three of the studies (Hong et al., 2015, Joosen et al., 2018)(Li et al., 2019), one study compared three groups (sedentary, exercise and comprehensive groups) based on different advice for activity (Knight et al., 2014), the participants were divided into four groups in one study for focal group discussion (Paul et al., 2017) while there was an exercise/training booklet control group in three studies (van Het et al., 2014, Kim and Glanz, 2013)(Muller et al., 2016), a waiting list control group in one study (Lyons et al., 2017) and a control group without specific exercise instruction in one study (Shake et al., 2018).
4.4. Usability and acceptance of interventions
Usability and acceptance of interventions were examined in three studies (van Het et al., 2014, Lyons et al., 2017)(Paul et al., 2017, Hong et al., 2015, Joosen et al., 2018). Lyons et al. (2017) found that the Jawbone Up app was usable in general older people and the acceptance rate was 80%, the app was considered user-friendly, convenient and comfortable in use by the participants. The participants also intended to continue use of the app in future.
Joosen et al. (2018) found that a smartphone-based solution is usable for monitoring PA in a care home. This system can monitor PA and present the level of PA in graphical form which can be translated into a fitness score. Furthermore, 58% of the participants consider the mHealth system beneficial to stay motivated for PA due to active monitoring. However, 74% of the participants asked for more encouragement to stay active in future.
Paul et al. (2017) reported on the acceptability and usability of the STARFISH app. In the pilot study, older people in focal group discussions gave positive comments on the acceptability and usability of the app for staying physically active. Many participants in the study found that the app was easy to understand and simple to use. The participants expressed that the app encouraged them to perform PA.
4.5. Effectiveness of interventions
Overall, eight out of ten studies found that mHealth interventions were effective on PA or exercise in older people irrespective of the kind of mHealth intervention (whether it was app-based, text message-based or mounted sensor-based for activity monitoring). In the studies of Knight et al. (2014) and Paul et al. (2017), the increase in step count for PA was not statistically significant. Further, the study of Joosen et al. (2018) reported the transient effect (increase in PA) of the mHealth system until the mid-period of the application of the intervention, when a motivation to use new technology was there. While the study of Muller et al. (2016) reported that PA behaviour diminished when the intervention was stopped.
Between group comparisons, next to ingroup comparisons, were made in six of the studies (van Het et al., 2014, Lyons et al., 2017, Knight et al., 2014, Kim and Glanz, 2013, Muller et al., 2016)(Shake et al., 2018). The between group comparisons have shown that the participants in the intervention groups improved more on PA in comparison to the control groups. Ingroup comparisons were made in all studies and participant improved on PA measures compared to baseline. Further details can be found in Table 2.
4.6. Motivational Reminders
One of the studies in our review reported a decrease in PA level after withdrawal of motivational reminders (Kampmeijer et al., 2016). It is difficult to say whether a single daily reminder is more effective than a reminder which is two or three times a day for optimal PA. In the studies, interventions were diverse which make a proper comparison difficult. The study on self-measured PA reported the efficacy of five different motivational text messages five times a week (Muller et al., 2016), similarly a study with three text messages (in the morning, afternoon and evening) three days a week also reported effectiveness on step count (Kim and Glanz, 2013). Furthermore, fortnightly email was found to be effective to improve PA in cancer patients (Hong et al., 2015). Similarly, interventions with daily reminders for exercises reported better results than no-reminder control groups (van Het et al., 2014).
4.7. Effectiveness in relation to form of mHealth
Comparison of the effectiveness of mHealth in relation to simple and complex form of mHealth on objective measurement of step count was inconclusive. A simple motivational text message intervention in the study of Kim & Glanz (2013) resulted in an increase of approximately 680 step counts in 6 weeks. Though, a complex mHealth intervention in the study of Lyons et. al. (2017) resulted in an increase of approximately 1100 step counts in 12 weeks. Due to the difference between studies in the intervention period and population characteristics, it is difficult to say whether the simplicity or complexity of mHealth interventions have an effect on PA or not. It is noticeable that none of the studies in our review compared a text message intervention with an app intervention to improve PA in older people.
5. Discussion
The results of the current review indicate that mHealth may be acceptable and may be an effective tool to increase PA or exercise in older people. Both simple and complex mHealth interventions may be effective. The interventions may be effective in comparison to no intervention or a non-mHealth intervention and the intervention period lasted for a short period of 1.5 to 3 months. However, not all studies had a randomized controlled design, some studies conducted pre- and postintervention measurements without a control group.
This review is different than the review on the effectiveness of eHealth by Muellmann et al. (2018) as it is specifically focused on mHealth and all participants are 55 years old or above in the included studies. Muellmann et al. (2018) reported the effectiveness of eHealth interventions for a short term and was inconclusive about the efficiency of eHealth in the long period of time. The findings of this review on mHealth are consistent with the findings of Muellmann et al. (2018) on eHealth.
5.1. Motivational support
Motivational support is considered as an important aspect of mHealth interventions to improve PA (Kampmeijer et al., 2016). Motivational reminders may be important in interventions, but the optimal frequency of these reminders is not clear yet. If WHO guidelines are followed, the recommended PA is at least 150 minutes a week (accumulative) that can be like 30 minutes a day and five times a week in healthy older people while older adults with poor mobility should exercise for at least three days a week (World Health Organization. Global Strategy on Diet, Physical Activity and Health. https://www.who.int/dietphysicalactivity/leaflet-physical-activity-recommendations.pdfua=1. Published, 2011). A reminder on three or five days a week seems an appropriate choice, but the frequency of reminders also depends on the personality type (sedentary or active), personal need and preference of the person using it. Future research could investigate the optimal frequency of reminders for an optimal PA in different older people.
5.2. Simple and complex forms of mHealth
It would be interesting to investigate differences in effectiveness between simple and complex forms of mHealth in the future. In the future, apps could be more prevalent in advanced regions like Europe, the USA and China where more people own a smartphone while text messages are a good solution in developing countries in Asia and Africa where mobile phones are more common than smartphones and text messages are not expensive. It may be investigated in future research whether a motivational text message may have the same effect as an app or a complex system of mHealth (with mounted sensor) in older people.
5.3. Optimal Step Count
Step count is the objective method of measurement of PA and the average step count in healthy older people may range from 2000 to 9000 and pedometer-based interventions could cause an increase of 775 step count (Tudor-Locke et al., 2011). The recommended (increase in) daily step count for good physical health in older people is not specifically operationalized yet. In fact, the increase in step count is operationalized for some physiological conditions. For example, an increase of 600 or more daily step count is related to a low risk of hospital admission in older patients of Chronic Obstructive Pulmonary Disease (COPD)(Demeyer et al., 2016). More research is needed to determine the recommended (increase in) step count for older people.
5.4. WHO on PA in bouts of 10 minutes
The WHO recommends aerobic PA in bouts of at least 10 minutes (World Health Organization. Global Strategy on Diet, Physical Activity and Health. https://www.who.int/dietphysicalactivity/leaflet-physical-activity-recommendations.pdfua=1. Published, 2011). However, the included studies in this review did not explicitly use the bouts of 10 minutes. This might be related to the fact that the activity performed in bouts of less than 10 minutes could be equally effective, as the recommendation of PA in bouts of 10 or more minutes is supported by limited data (Murphy et al., 2009, Glazer et al., 2013). Further, intensive exercises of short duration do not give so much health benefits, when there are long periods of sedentary behaviour (Chastin et al., 2011). In the future, the WHO may further investigate/elaborate its recommendation on PA for older people regarding the bouts of 10 minutes.
5.5. mHealth and Population groups
An effective PA intervention for the general population might need some adaptations to stay effective in the subgroups of that population(Boekhout et al., 2017). In older people, the effectiveness of the same mHealth interventions may vary in different subgroups based on age, educational status, digital literacy, ethnicity and cultural perspectives. So, older people may not be treated as a single group. In the future, it might be interesting to compare an intervention in different groups of older people.
5.6. Future of mHealth
The future of mHealth interventions for PA in older people looks promising. mHealth interventions have several benefits in comparison to traditional interventions. These benefits are related to low costs, the flexibility of time and place to work with the interventions, and the sustainability of mHealth interventions. Traditional interventions with coaching professionals are usually expensive and require a dedicated time and place. Further, a large number of older people that need PA interventions makes mHealth really promising.
6. Limitations
This review has certain limitations and its findings cannot be generalized due to reasons like small number of participants, heterogeneity of studied populations, absence of proper comparison between simple and complex forms of mHealth, short duration of interventions, no follow-up measurements, the inclusion of both RCTs and pre-post studies, low quality of some of the studies, inclusion of studies in which PA was just a part of an intervention for primary care or component for automatic monitoring and feedback, and the use of self-reported measures of PA in some of the studies.
In addition, studies were missing information on the participants’ education, digital skills and motivation to use mHealth. It might be that the results mainly account for a selective group of older people who are innovators or early adopters with good digital skills and motivation to adapt to change and use mHealth.
6.1. 2.8. Recommendations for future research
We recommend future research on the comparison of simple mHealth solutions with complex mHealth interventions. We recommend evaluation of the effectiveness of text message’ reminders delivered on a mobile phone compared to an app’ reminder. We suggest an investigation of the frequency of optimal reminders for PA. Only few studies were conducted on usability and acceptability of mHealth and more research is needed on it. Further research is recommended for evaluation of usability, acceptability and effectiveness of mHealth in older people in relation to digital literacy, physical health, socioeconomic status and follow-up of long duration.
7. Conclusion
To conclude, the results of this review suggest that mHealth may be effective to improve PA and show an increase in exercise behaviour in older people. Motivational reminders may be an important aspect of a good PA intervention. In the future, mHealth may add to or replace traditional methods of improving PA and it is necessary to tailor interventions with the needs of older people. Researchers could explore mHealth features which are precise, relevant, simple to use and still effective for maintaining and promoting good physical health. A large number of older people are in need of effective PA interventions and mHealth might be an economical and effective solution for their good physical health and independence in activities of daily life.
Uncited references
Gillespie and Gillspie (2012).
Acknowledgement
Special thanks to J. W. Schoones, Librarian at Waleus Library, Leiden University Medical Center, Leiden (The Netherlands) for his contribution to the literature search.
Funding Source
This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
Conflict of interest
Authors do not have any conflict of interest to declare.
References
-
D.E.R. Warburton, C.W. Nicol, S.S.D.BredinHealth benefits of physical activity: the evidence
Canadian Medical Association Journal., 174 (6) (2006), pp. 801-809
-
N.M. Peel, R.J. McClure, H.P.BartlettBehavioral determinants of healthy aging
Am J Prev Med., 28 (2005)
- World Health Organization. Global Strategy on Diet, Physical Activity and Health. https://www.who.int/dietphysicalactivity/leaflet-physical-activity-recommendations.pdf?ua=1. Published 2011.Assessed January 15, 2020.
-
F. Sun, I.J. Norman, A.E. WhilePhysical activity in older people: a systematic review
BMC Public Health., 13 (1) (2013), p. 449
-
W.A. Satariano, T.J. Haight, I.B.TagerReasons Given by Older People for Limitation or Avoidance of Leisure Time Physical Activity
Journal of the American Geriatrics Society., 48 (5) (2000), pp. 505-512
-
A.L. Dunn, B.H. Marcus, J.B. Kampert, M.E. Garcia, H.W. Kohl III, S.N.BlairComparison of Lifestyle and Structured Interventions to Increase Physical Activity and Cardiorespiratory FitnessA Randomized Trial
JAMA., 281 (4) (1999), pp. 327-334
-
J. Lahti, M. Laaksonen, E. Lahelma, O.RahkonenChanges in leisure-time physical activity after transition to retirement: a follow-up study
International Journal of Behavioral Nutrition and Physical Activity., 8 (1)(2011), p. 36
-
A.S. Slingerland, F.J. van Lenthe, J.W.Jukema, et al.Aging, retirement, and changes in physical activity: Prospective Cohort Findings from the GLOBE Study
Am J Epidemiol., 165 (2007)
-
D.A. Santos, A.M. Silva, F. Baptista, et al.Sedentary behavior and physical activity are independently related to functional fitness in older adults
Experimental Gerontology., 47 (12)(2012), pp. 908-912
-
K.A. Schutzer, B.S. GravesBarriers and motivations to exercise in older adults
Preventive Medicine., 39 (5) (2004), pp. 1056-1061
-
I.M.S.E. Lee, F. Lobelo, et al.Effects of physical inactivity on major non-communicable diseases worldwide: an analysis of burden of disease and life expectancy
In. Lancet, 380 (2012), pp. 219-229
-
M.L.P. Lindwall, M.S. HaggerThe reciprocal relationship between physical activity and depression in older european adults: a prospective cross-lagged panel design using SHARE data
In. Health Psychology, 30 (2011), pp. 453-462
-
J.A.P.-E.S. Ávila-Funes, S. Aguilar-Navarro, et al.Cognitive impairment and low physical activity are the components of frailty more strongly associated with disability
In. J Nutr Health Aging, 15 (2011), pp. 683-689
-
W. PtPhysical fitness and activity as separate heart disease risk factors: a meta-analysis
In. Med Sci Sport Exerc, 33 (2001), pp. 754-761
-
J.R.P.J. Sattelmair, E.L. Ding, et al.Dose-response between physical activity and risk of coronary heart disease: a meta-analysis
In. Circulation, 124 (2011), pp. 789-795
-
C.Y.L.R. Jeon, F.B. Hu, R.M. DamPhysical activity of moderate intensity and risk of type 2 diabetes: a systematic review
In. Diabetes Care, 30 (2007), pp. 744-752
-
E.M.E.S. Monninkhof, F.A. Vlems, et al.Physical activity and breast cancer: a systematic review
In. Epidemiology, 18 (2007), pp. 137-157
-
K.Y.Y.Y. Wolin, G.A. Colditz, I.M.LeePhysical activity and colon cancer prevention: a meta-analysis
In. Br J Cancer, 100 (2009), pp. 611-616
-
J.F.O. Woodcock, N. Orsini, I.RobertsNon-vigorous physical activity and all-cause mortality: systematic revie and meta-analysis of cohort studies
In. Int J Epidemiol, 40 (2011), pp. 121-138
- Gillespie LD RM, Gillspie WJ, et al. Interventions for preventing falls in older people living in the community. In. Cochrane Database of Systematic Reviews2012;9:Art. No.CD007146.
-
F.V.D. Sofi, D. Bacci, et al.Physical activity and risk of cognitive decline: a meta-analysis of prospective studies
In. J Intern Med, 269 (2011), pp. 107-117
-
M.E.R.W. Nelson, S.N. Blair, et al.Physical activity and public health in older adults: recommendations from the American College of Sports Medicine and the American Heart Association
In. Circulation, 116 (2007), pp. 1094-1105
-
W.J.P.D. Chodzko-Zajko, M.A. Fiatarone-Singh, et al.Exercise and physical activity for older adults. Position stand of the American College of Sports Medicine
In. Med Sci Sport Exerc, 41 (2009), pp. 1510-1530
-
A.E.R.R. Bauman, J.F. Sallis, et al.Correlates of physical activity: why are some people physically active and others not?
In. Lancet, 380 (2012), pp. 258-271
- World Health Organization. https://www.who.int/ehealth/about/en/. Published 2016. Assessed January 15, 2020.
-
T.L. Davis, R. DiClemente, M.PrietulaTaking mHealth Forward: Examining the Core Characteristics
JMIR mHealth and uHealth., 4 (3) (2016)
-
B.H. Marcus, D.M. Williams, P.M.Dubbert, et al.Physical Activity Intervention Studies
Circulation., 114 (24) (2006), pp. 2739-2752
-
J.-H. LeeFuture of the Smartphone for Patients and Healthcare Providers
Healthc Inform Res., 22 (1) (2016), pp. 1-2
-
G.A. O’Reilly, D. Spruijt-MetzCurrent mHealth Technologies for Physical Activity Assessment and Promotion
American Journal of Preventive Medicine., 45 (4) (2013), pp. 501-507
-
M. Gotsis, H. Wang, D. Spruijt-Metz, M.Jordan-Marsh, T.W. ValenteWellness partners: design and evaluation of a web-based physical activity diary with social gaming features for adults
JMIR research protocols., 2 (1) (2013)
- Sarasohn-Kahn J. California Health Care Foundation. How Smartphones Are Changing Health Care for Consumers and Providers. https://www.chcf.org/wp-content/uploads/2017/12/PDF-HowSmartphonesChangingHealthCare.pdf . Published 2010.Assessed January 15, 2020.
-
H. Geraedts, A. Zijlstra, S.K. Bulstra, M.Stevens, W. ZijlstraEffects of remote feedback in home-based physical activity interventions for older adults: a systematic review
Patient Educ Couns., 91 (1) (2013), pp. 14-24
-
A. Romeo, S. Edney, R. Plotnikoff, et al.Can Smartphone Apps Increase Physical Activity? Systematic Review and Meta-Analysis
J Med Internet Res., 21 (3) (2019), Article e12053
-
S.S. Coughlin, M. Whitehead, J.Q.Sheats, J. Mastromonico, S. SmithA Review of Smartphone Applications for Promoting Physical Activity
Jacobs J Community Med., 2 (1) (2016), p. 021
-
G. Flores Mateo, E. Granado-Font, C.Ferré-Grau, X. Montaña-CarrerasMobile Phone Apps to Promote Weight Loss and Increase Physical Activity: A Systematic Review and Meta-Analysis
J Med Internet Res., 17 (11) (2015), Article e253
-
S. Muellmann, S. Forberger, T. Mollers, E.Broring, H. Zeeb, C.R.PischkeEffectiveness of eHealth interventions for the promotion of physical activity in older adults: A systematic review
Prev Med., 108 (2018), pp. 93-110
-
N.H. Jonkman, K.S. van Schooten, A.B.Maier, M. PijnappelseHealth interventions to promote objectively measured physical activity in community-dwelling older people
Maturitas., 113 (2018), pp. 32-39
-
J.P.T. Higgins, D.G. Altman, P.C.Gøtzsche, et al.The Cochrane Collaboration’s tool for assessing risk of bias in randomised trials
BMJ., 343 (2011)
-
R.E. van Het, P. Silveira, F. Daniel, F.Casati, E.D. de BruinTablet-based strength-balance training to motivate and improve adherence to exercise in independently living older people: part 2 of a phase II preclinical exploratory trial
J Med Internet Res., 16 (6) (2014), Article e159
-
E.J. Lyons, M.C. Swartz, Z.H. Lewis, E.Martinez, K. JenningsFeasibility and Acceptability of a Wearable Technology Physical Activity Intervention With Telephone Counseling for Mid-Aged and Older Adults: A Randomized Controlled Pilot Trial
JMIR Mhealth Uhealth., 5 (3) (2017), Article e28
-
E. Knight, M.I. Stuckey, R.J.PetrellaHealth promotion through primary care: enhancing self-management with activity prescription and mHealth
Phys Sportsmed., 42 (3) (2014), pp. 90-99
-
B.H. Kim, K. GlanzText messaging to motivate walking in older African Americans: a randomized controlled trial
Am J Prev Med., 44 (1) (2013), pp. 71-75
-
A.M. Muller, S. Khoo, T. MorrisText Messaging for Exercise Promotion in Older Adults From an Upper-Middle-Income Country: Randomized Controlled Trial
J Med Internet Res., 18 (1) (2016), Article e5
-
L. Paul, S. Brewster, S. Wyke, et al.Increasing physical activity in older adults using STARFISH, an interactive smartphone application (app); a pilot study
Journal of rehabilitation and assistive technologies engineering., 4 (2017)
-
Y.A. Hong, D. Goldberg, M.G. Ory, et al.Efficacy of a Mobile-Enabled Web App (iCanFit) in Promoting Physical Activity Among Older Cancer Survivors: A Pilot Study
JMIR Cancer., 1 (1) (2015), Article e7
-
P. Joosen, D. Piette, J. Buekers, J.Taelman, D. Berckmans, B.P. DeA smartphone-based solution to monitor daily physical activity in a care home
J Telemed Telecare. (2018)
-
M.C. Shake, K.J. Crandall, R.P. Mathews, D.G. Falls, A.K. DispennetteEfficacy of Bingocize®: a Game-Centered Mobile Application to Improve Physical and Cognitive Performance in Older Adults
Games for health journal., 7 (4) (2018), pp. 253-261
-
J. Li, N. Hodgson, M.M. Lyons, K.C. Chen, F. YuGooneratne NS
A pilot feasibility study. Geriatric nursing, A personalized behavioral intervention implementing mHealth technologies for older adults (2019), p. 03
-
R. Kampmeijer, M. Pavlova, M. Tambor, S.Golinowska, W. GrootThe use of e-health and m-health tools in health promotion and primary prevention among older adults: a systematic literature review
BMC Health Serv Res., 16 (Suppl 5)(2016), p. 290
-
C. Tudor-Locke, C.L. Craig, Y. Aoyagi, et al.How many steps/day are enough? For older adults and special populations
The international journal of behavioral nutrition and physical activity., 8 (2011)
-
H. Demeyer, C. Burtin, M. Hornikx, et al.The Minimal Important Difference in Physical Activity in Patients with COPD
PLoS One., 11 (4) (2016)
-
M.H. Murphy, S.N. Blair, E.M.MurtaghAccumulated versus Continuous Exercise for Health Benefit
Sports Medicine., 39 (1) (2009), pp. 29-43
-
N.L. Glazer, A. Lyass, D.W. Esliger, et al.Sustained and shorter bouts of physical activity are related to cardiovascular health
Medicine and science in sports and exercise., 45 (1) (2013), pp. 109-115
-
S.F.M. Chastin, E. Ferriolli, N.A.Stephens, K.C.H. Fearon, C.GreigRelationship between sedentary behaviour, physical activity, muscle quality and body composition in healthy older adults
Age and Ageing., 41 (1) (2011), pp. 111-114
-
J.M. Boekhout, D.A. Peels, B.A.Berendsen, C.A. Bolman, L. LechnerAn eHealth Intervention to Promote Physical Activity and Social Network of Single, Chronically Impaired Older Adults: Adaptation of an Existing Intervention Using Intervention Mapping
JMIR Res Protoc., 6 (11) (2017), Article e230



